Hot Seat #89: 12mo with respiratory distress
Posted on: February 27, 2017, by : Jared Friedman
Jared Friedman MD, Inova Children’s Hospital
With Kathy Brown MD, Children’s National Medical Center
The Case
An 12 month old, full-term, NSVD, male without any PMH, presented with fever (TMax 101.6F), URI symptoms, and slightly decreased PO for 5-6 days. The parents noted “difficulty breathing” and “trying to catch his breath” which prompted the sudden visit to the Emergency Department. They saw the pediatrician 3 days prior to visit, who said there was an “infection” and started the patient on Amoxicillin at that time. The fever continued, however, and the patient was kept out of daycare.
ROS: The parents deny any vomiting, diarrhea, travels, sick contacts, changes in UOP, changes in mental/neurological status, or any other concerns.
PMH: Negative.
FHx: Mother and Uncle both have Diabetes Type 1.
PE:
Vitals: BP 102/71, HR 137, RR 54, T 101.4F, O2 98% RA
General: Alert, uncomfortable and in moderate respiratory distress being held in Dad’s arms.
HEENT: NCAT, PERRL/EOMI – no injected conjunctiva, clear nasal discharge, no nasal flaring. No obvious palpable lymphadenopathy. Mildly erythematous OP without any tongue/mouth swelling. Lips appear slightly red. No obvious drooling.
CVS: Tachycardic, RRR, +2 pulses x4
Resp: Coarse breath sounds and transmitted upper airway sounds. Subcostal and suprasternal retractions (RR 60 on exam). Intermittent stridor and hoarseness noted only with agitation.
Abd: Soft, NTND, no HSM
GU: Normal female external genitalia
Ext/Skin: WWP, CR<2 sec. No swelling at extremities noted.
Neuro: No gross changes.
Question #1:
Due to the stridor, the patient was initially treated for croup with Motrin, Decadron, and nebulized racemic epinephrine. The patient immediately vomited after the motrin and Decadron. Upon re-evaluation 15 minutes later, the patient was found to have worsening tachypnea and retractions. The repeat vitals showed sats at 97% RA, temperature 102F, heart rate 146, and unable to obtain another blood pressure.
Question #2:
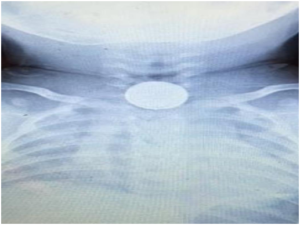
At this time, a STAT portable soft-tissue neck XR and CXR was ordered. A metallic foreign body with a double-rim consistent with a button battery was found on XR in the esophagus at the thoracic inlet.
The patient continued to have stridor with agitation and tachycardia, with slowly decreasing oxygen saturations (around 90% RA). You discuss the case with the on-call ENT, who agrees that the battery should be removed as soon as possible. They are preparing the operating room, which should be ready in about 15 minutes.
Question #3:
How would you approach this case? Please share your opinions by clicking on “What do you think?” below.
The information in these cases has been changed to protect patient identity and confidentiality. The images are only provided for educational purposes and members agree not to download them, share them, or otherwise use them for any other purpose.
Do you know where your crash airway supplies are and how to use them?
Would you ever attempt your own bougienage?
Talk tomorrow. Batteries… sigh.