Hot Seat #53 Denouement: 3 yo M p/w b/l knee swelling and refusal to walk
Posted on: March 26, 2015, by : Lenore Jarvis MD MEd
by Jaclyn Kline, Children’s National
with Mike Quinn, Children’s National
The Case
The case involves a previously healthy 3 yo boy presenting with fever, refusal to walk, b/l knee swelling and fever. It provides a great discussion of bilateral knee pain and swelling.
Here’s How You Answered Our Questions
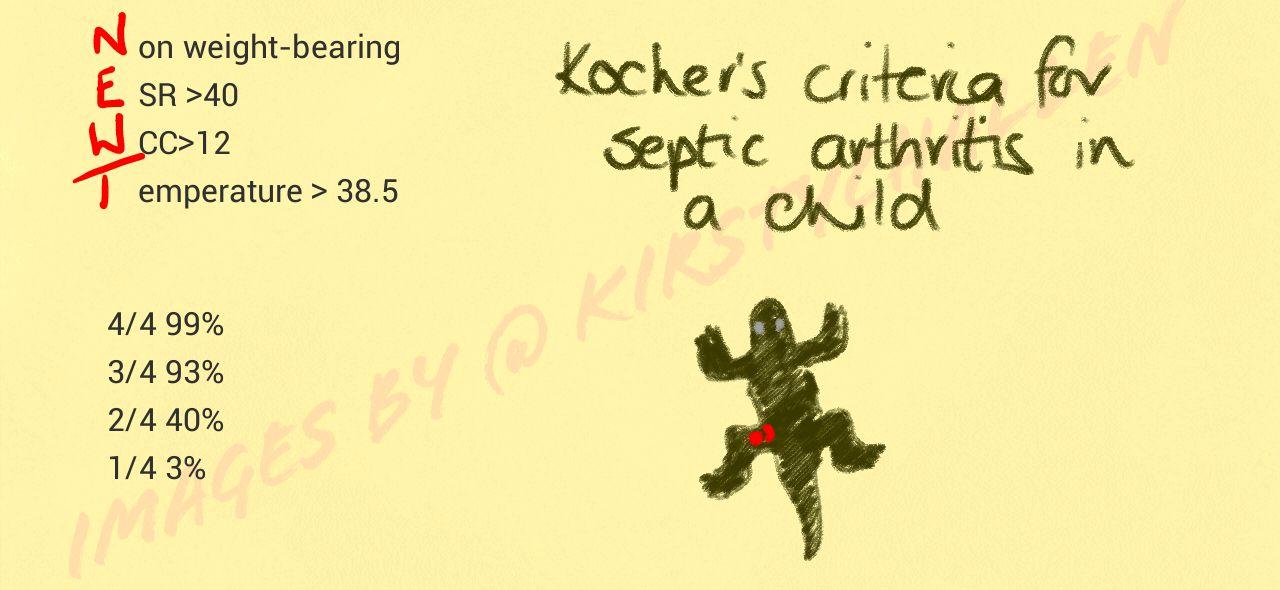
Many physicians felt that they should wait for the labs to come back prior to proceeding. Currently the patient is febrile (38 C) and non-weight-bearing. Several physicians mentioned waiting for the ESR & WBC and using the Kocher criteria to help guide further management on whether to tap the patient (although it would be rare to have septic joints in bilateral knees, and realizing that the Kocher criteria was created for hips). One should definitely send Lyme titers and recall that you don’t need to send Lyme titers from the knee fluid as blood is sufficient. With 2/4 Kocher criteria being met (however in bilateral knees), one could consult Ortho to see if a tap is warranted. Many ED providers felt comfortable tapping, but they weren’t sure that it was indicated. As the patient did not improve with NSAIDs, the more experienced providers felt that the patient should be admitted for further work-up. Several providers suggested consulting Ortho, Rheum and admitting to the Hospitalist Service for further care.
Denouement
Given fever and lab findings, septic arthritis was of concern in this case, although the bilateral symptoms were puzzling. Our patient met 2 of 4 of the Kocher Criteria (non-weight bearing, although bilaterally, and ESR > 40).
We consulted orthopedics in the ED, they evaluated the child and reviewed the labs, did not perform arthrocentesis in the department.
We admitted the child to the hospitalist service for further workup and symptomatic management, as child remained non-weight bearing. Remained off antibiotics after discussion with orthopedics and hospitalist teams with the working differential of: septic arthritis (although less likely given bilateral presentation in well-appearing child), Lyme arthritis, rheumatologic process, or toxic synovitis.
Day after admission, Lyme titer came back positive and ID was consulted, child was placed on course of oral amoxicillin to presumptively treat for Lyme arthritis. They also sent a workup including EBV and Parvovirus titers, which ultimately resulted negative.
The same day, he was taken to the operating room with orthopedics for bilateral arthrocentesis. Results of the fluid showed: 126,025 WBCs and 88,381 WBCs, 5,000 RBCs and 124,000 RBCs (unable to assess laterality on chart review). Sent for culture, but no microorganisms seen on smear.
After arthocentesis child comfortable and ambulating normally. He was discharged the following day to finish a course of amoxicillin. The culture of the joint fluid did not grow any organisms after 5 days of incubation. A PCR looking for Kingella kingae was also negative.
Teaching Points from Thursday Conference
Today we had a great discussion on the ddx of bilateral knee pain/swelling with fever: infectious, post-infectious, rheumatologic, heme/onc, trauma.
Citing Jennifer, “The biggest concern is septic joint. Using the Kocher criteria and acknowledging their limitations (retrospectively-derived parameters looking at the hip and not knee joint), the child could meet criteria for a knee tap, whether by ED provider or by Ortho colleague.”