Airway Adjuncts
Posted on: March 25, 2025, by : Haroon Shaukat MD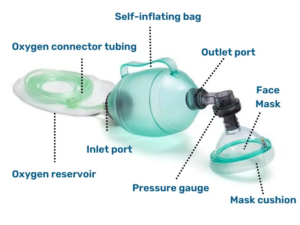
This session covers:
- General overview
- C-E hold
- Ensuring proper ventilation and oxygen delivery
- Oro-pharyngeal airways
- Naso-pharyngeal airways
A. Overview
Indications:
- Respiratory failure:
- Inadequate respiratory effort (apnea,hypoventilation)
- Ineffective breathing or severe respiratory distress
- Hypoxia unresponsive to supplemental oxygen
- Severe airway obstruction(as a temporizing measure)
- During resuscitation: Cardiopulmonary arrest or peri-arrest states
- Preparation for intubation: Preoxygenation or rescue ventilation during failed airway attempts
- Transport of unstable patients: To maintain oxygenation/ventilation
Contraindications:
- Complete upper airway obstruction (unless attempting to ventilate whilepreparing for definitive airway)
- Facial trauma/deformity or poor mask seal (use alternative airway management like supraglottic airway or intubation)
- High risk of aspiration with ineffective airway protection (consider early definitive airway)
- Note:There are no absolute contraindications if BVM is the only option to oxygenate a patient in extremis
Complications:
- Gastric insufflation: Risk of vomiting and aspiration
- Barotrauma: Pneumothorax or pneumomediastinum from excessive pressure
- Hypoventilation or hyperventilation: Leading to hypoxia or respiratory alkalosis
- Poor mask seal: Leading to inadequate ventilation and oxygenation
- Increased intracranial pressure (ICP): If hyperventilated in head injury patients
- Provider fatigue: In prolonged resuscitation efforts
B. Procedure for bag-valve mask ventilation:
Steps to Perform the C-E Hold:
- Position yourself at the patient’s head and adjust the height of the bed–
- Use your thumb and index finger (forming the “C”)to create a seal around the mask apex and sides.
- Apply gentle downward pressure to maintain the seal.
- Place your middle, ring, and pinky fingers (forming the “E”)along the bonymandible:
- Apply an upward lifting force to perform a jaw thrust.
- Avoid pressing on soft tissues of the neck to prevent airway obstruction.
- Ventilate using the bag with your other hand.

Key Tips:
- ✅ Maintain neck in sniffing position if no C-spine concern.
- ✅ Avoid excessive pressure that could occlude the airway.
- ✅ Ensure visible chest rise with each breath.
- ✅ If unable to get a good seal—consider two-person technique.
Video Demonstration:
Watch a Pediatric BVM Ventilation with C-E Hold (Video: Proper BVM technique, including C-E hold and jaw thrust demonstration)
C. Ensuring Proper Ventilation with BVM
How to Confirm Adequate Ventilation:
- Observe visible chest rise and fall with each ventilation.
- Monitor oxygen saturation (SpO₂) and heart rate—improvements suggest effective ventilation.
- Listen for bilateral breath sounds over lung fields.
- Avoid over-ventilation—deliver gentle, controlled breaths (~6-8 mL/kg tidal volume).
- Watch for gastric distention, which suggests air entering the stomach instead of the lungs.
- Tip: In small infants, use a manometer if availableto prevent high pressures (>20-25cm H₂O) that risk barotrauma.
⚠️ Pitfalls in Oxygen Delivery with a BVM (Ambu Bag):
- BVM does not provide passive oxygenation.
- Why? The self-inflating bag only delivers oxygen during active squeezing.
- Passive flow through the maskcannot occurbecause the bag’s valve preventsoxygen flow unless squeezed.
- If a patient is apneic but breathing is expected to resume, BVM alone is inadequate for apneic oxygenation—use high-flow nasal cannula or non-rebreather mask for passive oxygen delivery.
- Reservoir bag attachment is essential for delivering high FiO₂ (close to 100%).Without it, FiO₂ drops significantly.
- Mask leaks reduce effective ventilation and oxygenation.
✅ Take-Home Points:
- Chest rise is the most reliable signof effective ventilation.
- Self-inflating BVMs do not provide oxygen passively—oxygen is delivered only when the bag is squeezed.
- Always check equipment setup:
- Oxygen tubing connected and running at10-15 L/min
- Reservoir bag attached and filled
- Proper mask size and seal
Airway Adjuncts
D. Oropharyngeal Airway (OPA):
Indications:
- Unconscious patient without a gag reflex
- Airway obstruction from tongue or soft tissue collapse
- To facilitate effective BVM ventilation
Contraindications:
- Concious or semi-conscious patients (intact gag reflex -> risk of vomiting/aspiration)
- Oral trauma or mandibular fracture
Sizing and Insertion:
- Measure: From the corner of the mouth to the angle of the mandible.
- Insertion:
- Option 1 (older children): Insert upside down, then rotate 180° once past the tongue.
- Option 2 (infants/small children): Insert right-side up using a tongue depressor to avoid trauma.
- Ensure the flange rests against the lips and airway is patent.

Video: OPA Insertion Demo (Pediatric) Watch Here
E. Nasopharyngeal Airway (NPA):
Indications:
- Semi-conscious patients or those with intact gag reflex needing airway support
- BVM ventilation where OPA is contraindicated
- Oral trauma, clenched teeth, or seizure activity
- Sizing and Insertion:1.Measure:From thetip of the nose to the tragus of the ear.2.Insertion:a.Lubricate the airway with water-based gel.b.Insertbevel toward the septumalong the floor of the nostril.c.Advance gently until the flangerests against the nostril.3.If resistance is met, try the other nostril.
Contraindications:
- Basilar skull fracture or facial trauma(risk of intracranial placement)
- Coagulopathy or nasal obstruction
Sizing and Insertion:
- Measure:From the tip of the nose to the tragus of the ear.
- Insertion:
- Lubricate the airway with water-based gel.
- Insert bevel toward the septum along the floor of the nostril.
- Advance gently until the flange rests against the nostril.
- If resistance is met, try the other nostril.

Video: NPA Insertion Demo – Watch Here
⚠️ Pro Tips:
- Choose the largest size that fits comfortably to minimize airway resistance.
- Reassess airway patency and chest rise after placement.
- Both adjuncts do not replace definitive airway management if needed.
