Hot Seat #187: Why won’t he eat?
Posted on: March 20, 2022, by : Dennis RenCase by: Dennis Ren, MD

HPI: A 5-year-old boy presents to the ED refusing to eat. He had an episode 5 days ago when he choked on a meatball while eating. Parents state that spit the meatball out in its entirety. Since that time, he has been extremely anxious about eating. His parents have offered him a variety of foods, but he has still refused to eat. He is still drinking and has had a normal urine output. He has not had any abdominal pain or change in bowel habits during this time.
Review of Systems:
Constitutional: + decreased energy
HEENT: Denies congestion, rhinorrhea,
RESP: Denies SOB, cough
Cardiovascular: Denies chest pain, palpitations, syncope
GI: Denies abdominal pain, vomiting, diarrhea
GU: Normal urine output
PMHx/PSHx: No past medical or surgical history. Does not take any medications.
FamHx: No GI disorders. No eating disorders
Social: Lives with parents.
Physical Exam:
Vitals: T: 36.9 C HR: 116 RR: 20 BP: 125/79 O2: 99% on room air
General: Alert, withdrawn, tired-appearing, answers questions.
Skin: Warm, dry, intact, no rash
Head: Atraumatic
Neck: Supple, no LAD
Eyes: PERRL, EOMI, normal conjunctiva
Ears, Nose, Mouth, and Throat: Moist oral mucosa. No pharyngeal erythema, exudates, or evidence of trauma. TMs clear
Cardiovascular: Regular rate and rhythm. No murmurs. No rubs. No gallops. <2 second capillary refill
Respiratory: CTAB. Non-labored respirations
GI: Soft, nontender, non-distended.
MSK: No swelling. No tenderness. Moves all extremities
Neurological: Alert. Normal motor and coordination observed.
Case continued…
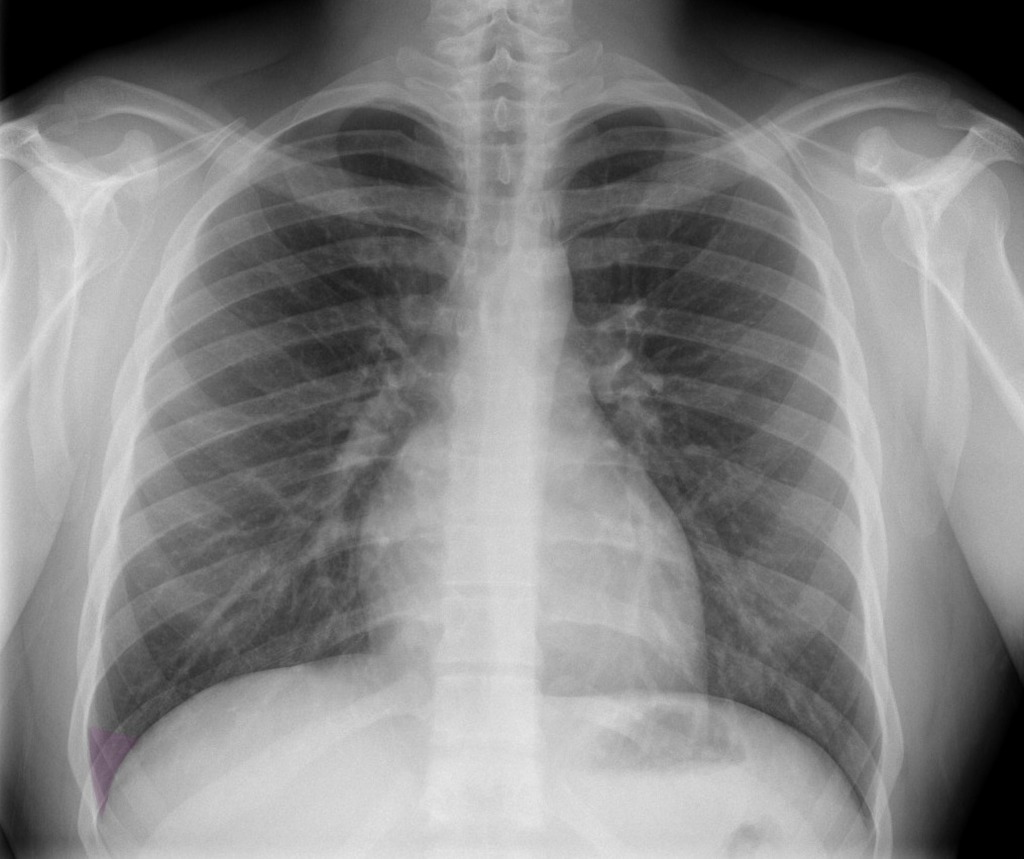
You obtain a foreign body XR (shown below). You offer the patient multiple options for food and drink in the ED. He takes one bite of his favorite crackers and sip of water and then stops. No apparent throat pain noted. No episodes of abdominal pain or vomiting.
Imaging (read as normal):

On repeat exam you find:
Vitals: Afebrile, HR- 112, RR- 16, BP: 94/71, SaO2- 99% @RA
Gen: No distress, lying comfortably in bed
HEENT: no erythema, swelling
Pulm: No stridor or wheeze
Ab: soft, NTND
The information in these cases has been changed to protect patient identity and confidentiality. The images are are only provided for educational purposes and members agree not to download them, share them, or otherwise use them for any other purpose.

Once this child failed to have significant PO in the ED with encouragement, he needs a definitive study like an Upper GI to rule out any narrowing. Had a teen come in for what seemed like just food refusal at midnight on a Friday and ended up with a terrible stricture from eosinophilic esophagitis. She looked as good as this kid is presented. And I would really struggle with sending this kid home if he is not taking any solid foods. Admit to hospitalist, get the upper GI, have speech work with him once cleared if this is all coming from free of choking.
The sudden onset of food refusal after the inciting event of choking fits well with ARFID. The ddx to consider is food impaction (though kids usually can feel the stuck feeling in the chest), retained foreign body, stricture, GERD, EE, IBD. The lack of other symptoms such as chest pain or vomiting makes ARFID more likely. Given the short duration of symptoms, no workup is needed in the ED. If it were more longstanding, the labs typically done for patients with restrictive eating disorders would be indicated. Before discharge, it is important to have a tight follow-up plan with the PMD or with other subspecialists to address the disordered swallowing and the anxiety (Adolescent Medicine may have good recommendations, even though this is a younger child).
This child presents with acute food refusal after a choking incident. He is also demonstrating some systemic symptoms with fatigue. Although the meatball was “intact” was there a secret second meatball? Or was the choking incident an “iceberg above the surface” and has this child been slowly having difficulty swallowing the whole time. We may never know, however with failure of PO challenge in the ED it behooves us to make sure there is not esophageal narrowing or obstruction. With his good tolerance of PO liquids he should be able to follow up with the appropriate team at discharge whether it be GI, PMD, or PCP.