Hot Seat #195: 10-month-old with diarrhea
Posted on: September 20, 2022, by : Harrison Hayward
10-month-old ex FT F presents with subjective fever and bloody diarrhea. Patient with 3 days of non-bloody diarrhea, however, 1st day of bloody diarrhea was day of ER presentation. Caretaker describes it as bright red streaks of blood and mucus mixed in with stool. Caretaker is unsure of stool frequency but approximates it’s with every feed and each diarrheal episode today has had blood. Yesterday, patient felt warm with axillary Tmax of 100 for which she’s received Tylenol. Denies anyone in the family having similar symptoms. Reports 1 episode of NBNB emesis 3 days ago with no recurrence. Denies change in eating patterns. Shares it’s difficult to discern pure wet diapers as patient is having frequent diarrheal episodes. Endorses concurrent cough/URI symptoms. Patient recently returned from an international trip 6 days ago. Denies patient having rash, rigors, diaphoresis, irritability, jaundice, or changes in color of urine. Denies patient receiving malaria prophylaxis. While abroad reports being in an urban environment, primarily indoors, denies mosquito bites or family members with fever or reports of malaria.
ROS
Constitutional symptoms: no fever.
Skin symptoms: denies rash.
Eye symptoms: no scleral icterus, denies discharge.
ENMT symptoms: Nasal congestion.
Respiratory symptoms: Cough, denies shortness of breath, denies wheezing.
Gastrointestinal symptoms: Vomiting, bloody diarrhea.
Neurologic symptoms: no altered level of consciousness.
Hematologic/Lymphatic symptoms: no bleeding tendency
Allergy/immunologic symptoms: no recurrent infections
PMH: ex FT, healthy, no developmental concerns
PSH: none
Meds: multi-vitamin
Allergies: none
Immunizations: up to date
Exam
Vitals: T-39.5, HR-180, RR-48, BP- 94/67, 100% on RA
General: Alert. appropriate for age. Playful with parent. Cries w/ examiner.
Skin: Warm, dry, pink, no rash or irritation in diaper area.
Head: Normocephalic, atraumatic.
Neck: Supple, no lymphadenopathy.
Eye: Normal conjunctiva, no discharge, no scleral icterus, +tears
Ears, nose, mouth and throat: Tympanic membranes clear. Oral mucosa moist.
Cardiovascular: Tachycardic. Normal rhythm. No murmur. Extremity pulses equal. Cap refill brisk.
Respiratory: Lungs are clear to auscultation. respirations are non-labored. breath sounds are equal.
Gastrointestinal: Soft. Nontender. Non distended. Normal bowel sounds. No organomegaly.
Genitourinary: Normal genitalia for age
Musculoskeletal: Normal ROM. normal strength. moves all extremities.
Neurological: No focal neurological deficit observed. Normal motor/sensory. Developmentally normal.
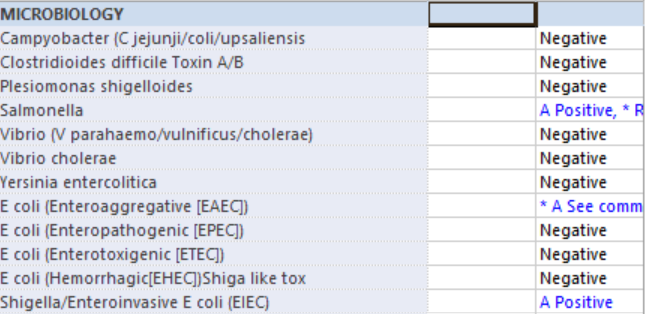
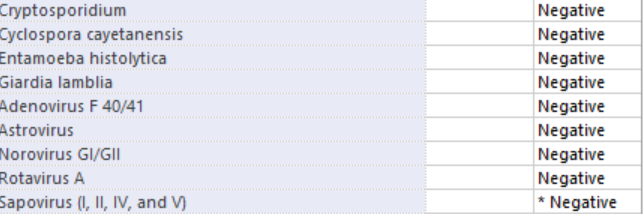
Given history there was lower concern for malaria. Due to being well appearing and clinically hydrated on exam, no labs were obtained. Regular diet was encouraged. Patient received PO Tylenol, however cried during administration causing NBNB emesis. Re-attempted Tylenol administration. GI Pathogen PCR and culture sent.
Repeat vitals T-37.6, HR 128, RR 40. Stool sample obtained. Patient tolerated snacks and formula with no emesis. Discharged home.

The patient was highly febrile and tachycardic on the first visit with unclear uop. I might have considered watching for improved vs or UOP, though it sounds like the patient was very well appearing. It would also be helpful to know where the patient traveled to as this can influence antibiotic resistance patterns as well as considerations for malaria.
Agree w Jill about location of travel being important regarding empiric antibiotic choice and risk stratification for malaria. If high risk location (regardless of urban/rural and known bites) I would have also checked basic labs and malaria smear. With questionable urine output and tachycardia, I might have also checked either urine or CBC/BMP to screen for signs of HUS. In older kids with bloody diarrhea, normal BP and a urine without heme/blood and no protein are reassuring and blood work might not be necessary, but in a baby with frequent diarrhea this might not be as practical. Re stool pathogens, age 6 mo with no other risk factors and well appearing, I do not always treat. Shigella treatment is also determined by level of illness; and risk of spread; it also decreases duration of symptoms and shedding. With high fever, age <12 mo, very frequent diarrheal stools, I'd treat in this case.
I actually just had a board practice question with similar presentation except that the patient was under 6 months so the immediate answer was to treat. My inclination with a child <1 with a bloody febrile diarrhea though wouod be to treat given the increased risk of bacterial translocation and sepsis But I also might be skewed given tge number of infants I saw this year with salmonella bacteremia