Hot Seat #216: Dazed and Confused
Posted on: October 9, 2023, by : Brandon Ho
Case by Erin Thomas MD, INOVA PEM Fellow
13-year-old transgender male with history of asthma, MDD, GAD, PTSD, h/o SI who presents with a seizure-like episode at school. He had 1 minute of witnessed convulsive seizure activity. Per mom, he was his normal self this morning. All medications were kept under lock and key at home due to previous suicide attempts. Mom does not believe any doses are missing.
He was brought in by EMS, anxious with slightly slurred speech but answering questions appropriately. He denied ingestions, trauma, or recent illness. Thirty minutes after arrival he developed tachycardia fluctuating between 115-175. He started to require assistance with transfer from bed to commode due to ataxic gait. He was noted to be inattentive, more confused, speaking nonsensically, and requiring frequent redirection.
EXAM:
Vitals: T 37.7C, HR 118, BP 146/91, RR 32, SpO2 98%
General: confused, jittery, delirious but redirectable
HEENT: normocephalic, atraumatic, dilated pupils, dry mucous membranes
CV: tachycardia, no murmur, cap refill <2 sec
Pulm: CTAB
Abdomen: full, soft, non-tender
MSK: normal ROM, no rigidity or tenderness
Skin: dry
Neuro/Psych: disoriented, anxious, jittery, no clonus
Bedside POCUS demonstrated significant urinary retention.
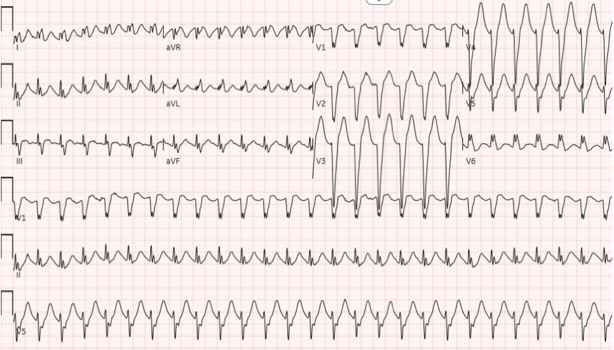
EKG showed:
Repeat vitals: Temp 38.4C HR 160 RR 34 BP 147/73 SpO2 98%
Patient was given multiple doses of sodium bicarbonate, Ativan, and 2g of magnesium sulfate. Toxicology workup was sent.
He was admitted to the PICU but continued to board in the ED until a bed was ready. Several hours later, he progressed to pulseless Vtach. He received 2 rounds of CPR, epinephrine, calcium, sodium bicarb and magnesium. ROSC was obtained and he was electively intubated. On review of telemetry, clear rhythm deterioration to torsades de pointes was noted.
