Hot Seat #42 Denouement: 17 year old girl who “passed out”
Posted on: September 11, 2014, by : Katie Donnelly MD
by Katie Donnelly, Children’s National
with Shilpa Patel, Children’s National
The Case
17 year old female who emigrated from El Salvador eight months ago who presents after an episode where she lost consciousness and had vision changes. The challenge in this case is how to approach this patient with recent travel history who is asymptomatic at presentation. For a complete case presentation with audience and Hot Seat Attending comments, please click here.
Here’s How You Answered Our Questions
Everyone wanted to get some form of imaging in this patient and the ratio of CT to MRI in both groups were the same.
What’s interesting was that fellows and newer faculty were more likely to do further interventions while our more experienced colleagues were content to admit to the PICU for close monitoring.
Denouement
Neurology was consulted in the Emergency Department, and with her new neurologic complaint she was admitted to the PICU for close monitoring and frequent neuro checks. There was suspicion that this syncopal episode had actually been seizure activity. Given the results of her head CT, a subsequent MRI was performed.
Given the CT/MRI results and recent emigration from Central America, a presumptive diagnosis of neurocystocercosis was made. Further questioning revealed that while the patient lived in El Salvador her main source of protein was pork cooked over a charcoal grill. Her blurry vision improved spontaneously and an exam by ophthalmology ruled out optic involvement. Initial treatment was to be albendazole and steroids, however there was difficulty in obtaining albendazole and the drugs represented a significant financial burden for the patient, so patient received one day of high dose praziquantel, which is an off label treatment in the United States. She was observed one additional day and had no complications from inflammation secondary to treatment. She was discharged home on a steroid taper. She was seen in follow up in neurology clinic one month later and had had resolution of her headaches and no recurrent syncopal/seizure episodes.
Debrief Teaching Points – from Thursday Conference
1. CT vs MRI: There was no good consensus on which study would be the better initial test for the asymptomatic patient. Once the patient had acute vision changes, however, everyone opted for an emergent CT as the study of choice
2. Concerning findings in this patient were the worsening headache and requiring CPR. Those two were “red flags” that pushed providers into ordering imaging, rather than evaluating this as run of the mill syncope.
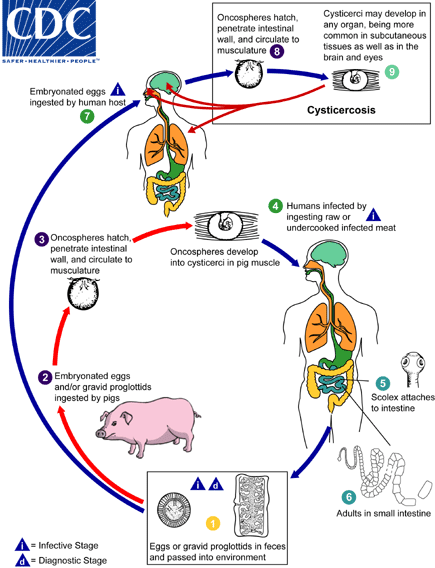
3. As Shilpa stated in her hot seat, you don’t technically get neurocystocercosis from ingesting undercooked pork. If you ingest pork infected with cyst, you develop GI disease and shed worms in your stool. Then you ingest the live worms via fecal-oral and poor water sanitation, which leads to cyst formation in the body. See the CDC image below for the complete life cycle.